LIVER CIRRHOSIS
What is End stage liver disease (ESLD) or Cirrhosis?
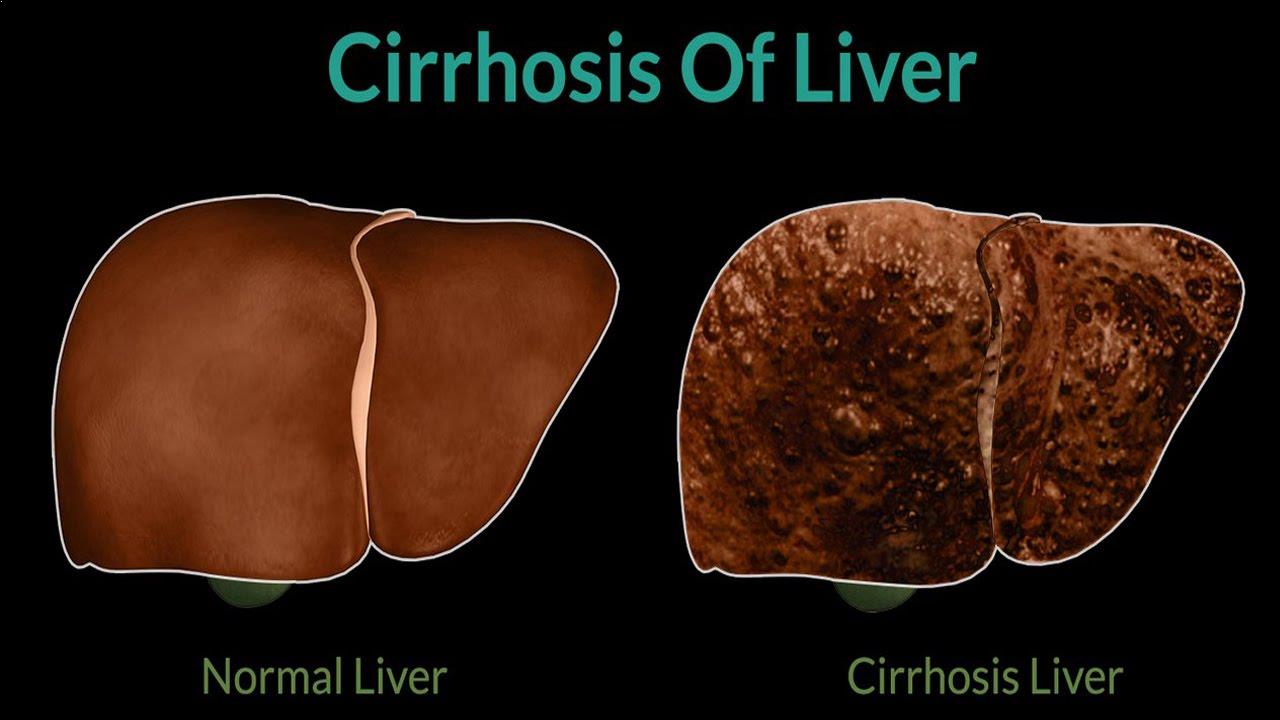
- Cirrhosis is a slowly progressing disease in which healthy liver tissue is replaced with scar (fibrous) tissue, causing loss of liver function.
- Cirrhosis liver loses its capacity to regrow or regenerate.
- The scar tissue affect the flow through the liver leading to back pressure changes in the blood vessels which bring blood to the liver. This is called as portal hypertension.
What Causes Cirrhosis (Scarring) of the Liver?
- Cystic Fibrosis
- Glycogen storage diseases
- Alpha 1 antitrypsin deficiency
- Hemochromatosis and Wilson’s diseases
- Blockage of the bile duct – Primary biliary atresia in infants/children.
Chronic alcohol ingestion
The heavier the drinking, the higher the risk of developing cirrhosis. About 1 to 10 heavy drinkers will eventually develop cirrhosis after 10 or more years of heavy drinking. Women who are heavy drinkers seem to be more prone than men to develop cirrhosis.
Chronic viral infections
Chronic viral infections of the liver (Hepatitis types B & C) usually takes about 15-20 years or even longer from the initial infection.
Non-alcoholic steatohepatitis (NASH)
Obesity and diabetes cause fat build up in the liver & increases the risk of developing NASH. This is an emerging cause of liver cirrhosis in western countries, now seen with increased frequency in India also.
Repeated Bouts of heart failure with fluid backing up into the liver.
Certain inherited diseases such as:
How common is cirrhosis?
There are an estimated 50,000 people living with cirrhosis in India and at least 7000 new cases being diagnosed every year. This number seems to be rising.
What are the Signs & Symptoms of liver diseases?
In the early stages of the condition, there may be no symptoms.
Human body may work well with up to 30% of the functioning liver parenchyma.
However as more & more liver cells get replaced by scar tissue, End-stage Liver diseases sets in & following sign & symptoms may develop:
- Yellowing of skin and white portion of the eyes (jaundice) or passing dark yellow urine.
- Fluid retention (edema) and swelling in the ankles, legs, and abdomen (after an early sign).
- Excessive sleepiness, inability to sleep, becoming forgetful, drowsy or confused (Hepatic Encephalopathy).
- Bloody vomiting, passing tarry black stools or blood in stools
- Clay coloured stools
- Loss of appetite
- Lack of energy (fatigue)
- Unintentional Weight loss
- Easy or excessive bruising
- Constant & severe itching (pruritus) all over the body
- Unexplained fever
Occurrence of above symptoms is called as decompensation & generally indicates poor or inadequate liver function or failure of medical therapy
Liver transplantation may be needed for patients with decompensated cirrhosis.
How is cirrhosis diagnosed?
- Symptoms and Clinical examination
- Blood tests
- An ultrasound Scan (CT scan or MRI scan)
- Liver Biopsy
What is the treatment for Cirrhosis?
Scarring of the liver or cirrhosis tends to get progressively worse if the underlying cause persist and is not treated. In general, once the damage is done the scarring is irreversible. The aim of the treatment is to prevent further liver scarring or to slow the progression of the scarring process.- Stop drinking alcohol
- Be cautious while taking medicines
- Symptomatic treatment:
- Adequate food intake & regular exercise
- Treatment of bleeding varices: A bleed from ‘swelled’ blood vessel (due to back pressure changes) is a medical emergency. Seek immediate medical help if
- You vomit blood
- You pass black coloured stool
- You pass blood in stools
- Drainage of fluid that builds up in the tummy (ascites)
- Medicines to reduce portal pressure
- Medicine to reduce itching
- Low –sodium diet & diuretics to reduce fluid accumulation in the body
- Vaccination for protection against Influenza & Pneumococcal infections.
Management of ESLD and its multi – system effects is complex and requires the expertise of a group of health care professionals including several doctor and trained staff who have special training & experience.